
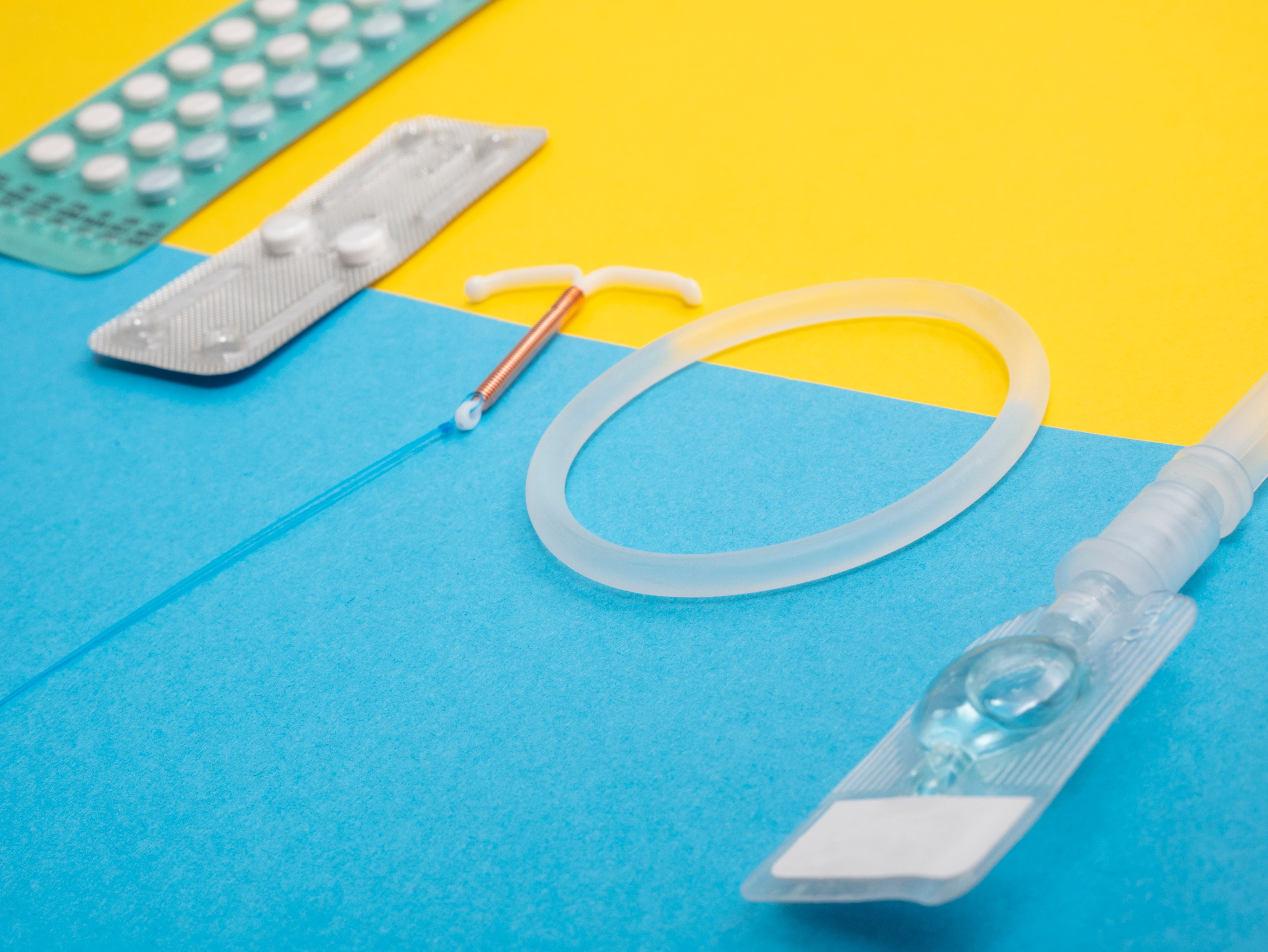
One of our main priorities is to ensure universal access to, and informed use of effective contraception. Millions of people lack the knowledge and information to determine when or whether they have children, and they are unable to protect themselves against sexually transmitted infections (STIs).
Articles about Contraception

What is pre-ejaculatory fluid (also known as pre-cum), and can it cause pregnancy?
There’s a good chance that you’re reading this because you are unsure of what pre-ejaculate (also known as pre-cum) fluid is, and if it can cause pregnancy. If you regularly use withdrawal as a contraception method, pre-ejaculate fluid is something you may want to know more about, especially if you are not planning a pregnancy or are worried about HIV and STIs. Read a quick round-up on the important things you should know about pre-ejaculate fluid. You can also watch our short animation on the effectiveness of the withdrawal (or ‘pulling out’) method. Pre-ejaculate is a natural lubricant Pre-ejaculate is a fluid that is discharged from a penis when it’s aroused and usually occurs right before ejaculation. The fluid acts as a natural lubricant during sex. It contains sperm Even though pre-ejaculate fluid comes from the ‘Cowpers gland’ (and not from testes like semen), some fluid can contain live sperm. A number of researchers believe this is a ‘cross-contamination’ from semen that may be present in the urethra from a previous sexual encounter, as both the pre-ejaculate fluid and semen pass through the urethra. It can cause pregnancy Although the chances of pregnancy from pre-ejaculate fluid is relatively low and can vary from person to person, 27% of those who use withdrawal as a regular form of contraception end up with a pregnancy. It can transmit STIs, including HIV Pre-ejaculate fluid can carry bacteria and viruses. Using the withdrawal method will not protect you from STIs, including HIV. If you are unsure of your partners’ status, consider another form of contraception. Men cannot control when it happens Most men cannot tell when they have pre-ejaculated. Withdrawal takes a lot of self-control, and in the heat of the moment, that can be a little difficult! So if you want to reduce the risk of STIs and HIV, and you’re not planning a pregnancy, you may want to use alternative contraception methods like the external condom or an IUD. To find out more about alternative contraception methods available to you visit our online guide to find the right option for you.

New flagship health programme to transform the lives of millions of women and girls
The lives of millions of women and girls will be transformed by new sexual and reproductive healthcare programmes led by International Planned Parenthood Federation (IPPF) and Marie Stopes International (MSI) consortia across Africa and South Asia. The programmes will launch integrated healthcare expansion in 27 countries and were announced in Kigali at the International Conference on Family Planning today. The Women’s Integrated Sexual Health (WISH) programme is funded by the UK Department for International Development (DFID), to deliver access to life-saving contraception for six million couples per year. The Secretary of State for International Development, Penny Mordaunt said: "Investing in family planning gives women control over their own bodies and lives. It helps them complete their education, pursue job opportunities and challenge inequality around the world." The new programme will accelerate progress towards meeting global commitments on expanding access to contraception made by governments and civil society organisations through the Family Planning 2020 (FP2020) movement. The IPPF and MSI WISH consortia will ensure previously unreached people, especially young and poorer women, are able to access contraception and have the choice on whether, when and how often to have children. IPPF’s Director General Dr Alvaro Bermejo said the WISH programme would transform lives. He said: "This is a significant investment and a deep commitment to putting women at the heart of healthcare. Women and girls – of all ages, places, income and education – must have access to high quality, voluntary family planning care and information. We thank the UK Government for their commitment to this vital issue. Together, we can accelerate change by expanding integrated healthcare through our clinics and outreach services. More services, wider contraceptive options and better access to safe abortion, means the right care at the right time. More power for every girl and woman to decide what to do with her body, with her life, and with her future." The WISH programme will scale up efforts at country level, expanding reach to millions of new users of sexual and reproductive health services. Genet Mengistu, the Executive Director of the Family Guidance Association of Ethiopia (FGAE), an IPPF member, said: "This is an incredible opportunity to accelerate change for women and girls to decide their own futures. It will get family planning services to Ethiopian women, particularly to those underserved." Simon Cooke, CEO at MSI, said: "Through this funding, we and our partners will be able to bring quality sexual and reproductive health services to millions of women in some of the world’s poorest and most marginalised communities. For many, it will be their first chance to access any kind of contraception, empowering them to stay in education, forge a career, stay healthy and pursue their hopes and dreams for the future. With this landmark investment in women and girls, the UK Government is creating the right conditions to drive multiple other areas of development, from increasing the number of girls completing education to enabling couples and families in poverty to maximise their earning potential. We applaud DFID for its continued support for this vital and life-changing work." The £200 million investment to leading sexual and reproductive health service providers IPPF and MSI is made-up of two individual DFID WISH awards, through consortium arrangements. Lot 1 is a consortium managed by MSI with 7 of its country programmes and 6 IPPF Member Associations, with a focus on West and Central Africa. Lot 2 is a consortium managed by IPPF with 16 Member Associations and 8 MSI country programmes with a focus on East and Southern Africa and Asia.
IPPF welcomes UNFPA's State of the World Population 2018 report
The UNFPA's State of the World Population report highlights that, while much progress has been made globally in upholding reproductive rights, there remains large inequalities in access and high levels of unmet needs. By grouping countries into low, medium and high fertility countries, the report recognizes the diverse needs globally, and the importance of targeted interventions. In high fertility countries, the high unmet need for family planning is one of the most important issues that governments and SRHR partners need to address by ensuring access to quality, rights-based contraceptive services. In low fertility countries, the report highlights infertility and needs of the ageing population - more needs to be done to prioritize these issues, especially in countries with low fertility. In countries with mid fertility, high adolescent fertility is a concern, and reflects the need to further strengthen youth friendly services, including comprehensive sexuality education. IPPF supports the report and especially its emphasis and recognition of the reproductive rights of couples, including the right to choose, the right to decide the number of children they wish to have and when, throughout the report. IPPF joins its voice with UNFPA and partners to call on governments to sustain their commitments to SRHR and ensure access to the full range of high quality universally accessible SRH services and allocate domestic funding to ensure that gender equality and sexual and reproductive rights are realized. This is of critical importance as the 25th anniversary of the historic commitments adopted by 179 governments in the Programme of Action of the International Conference of Population and Development in Cairo in 1994. IPPF aligns with the call made by the report on the rights of all women to choose and decide freely and without question over their bodies, sexuality and reproduction as a priority to achieve the agenda 2030.

World Contraception Day: Contraceptive funding in crisis
On this World Contraception Day, some 214 million women and girls in developing regions have an unmet need for modern contraception. These are women and girls who want to avoid a pregnancy but are not using a modern method of contraception. While the reasons for this are multiple, the costs and availability of contraception remain major barriers. Access to contraception is a basic human right. Governments affirmed women’s right to have access to safe, effective and affordable methods of contraception of their choice 24 years ago, at the International Conference on Population and Development in Cairo. In 2015, in the landmark Sustainable Development Goals, governments pledged to ensure universal access to family planning by 2030. Yet, three years on, global funding for contraceptives is in crisis. There is a major gap between needs for funding for contraceptives and the resources provided by both domestic and donor governments. In low- and middle-income countries out-of-pocket payments by individuals account for more than 80% of all spending on contraceptives. Domestic governments only provide around 8% of spending, while donors fund 10%. Out-of-pocket spending is an inequitable form of financing health services. Those least able to afford it carry most of the cost burden. The impact on household finances exacerbates inequalities and pushes people further into poverty. The gender implication is huge. Women and girls rely heavily on access to contraceptives and reproductive healthcare, and yet many do not have the financial means. Demand for contraceptives is expected to increase, which will further widen existing funding gaps. Estimates of the difference between today’s spending on contraceptives and the cost of meeting projected needs in low- and middle-income countries in 2020 show an additional funding gap of US$290m if current trends in use continue. Unless domestic or donor government finance increases substantially, most of this gap will have to be met by relying on user fees. Domestic governments have the main responsibility for ensuring access to contraception, yet donors continue to play an important role, particularly in the world’s poorest countries. In the 31 lowest income countries, donors currently finance 65% of all contraceptives, while domestic governments fund 7%. Individuals’ out-of-pocket spending accounts for 28%. Yet, while donor funding remains essential, it has faced a downward trend in recent years. Funding from the United States, the largest family planning donor, has been fairly stable but is now at risk. Funding pledges made by European and other donors in 2017 in support of the She Decides initiative and at the July London Family Planning Summit are promising, but it is too soon to tell whether they will bring a reversal in longer term funding trends. Domestic governments must live up to their responsibility to increase their funding and ensure access to contraception and healthcare. Yet, donors must also continue and step up their support. Millions of women and girls depend on it. - Raffaela Dattler, Financing for Development Advisor, IPPF
Integration of DMPA‑SC into the method mix contributes to increased uptake of all methods of family planning
Injectable contraceptives are an increasingly popular method of family planning. They are safe, discrete, highly effective, and generally last for several months. Sayana® Press, also known as subcutaneous depot medroxyprogesterone (DMPA‑SC), is a lower‑dose formula version of the already popular injectable Depo‑Provera. DMPA‑SC combines the drug and needle in a single‑use unit, which makes it easy to transport and simple to use with little training. DMPA‑SC can be administered by community health workers (CHWs) and women themselves – potentially making injectable contraceptives available to women who can’t easily travel to clinics.
IMAP Statement on emergency contraception
Emergency contraception (EC) refers to any contraceptive method that can be used after having unprotected or inadequately protected sexual intercourse (UPSI) but before pregnancy occurs, providing women with the opportunity to prevent an unwanted pregnancy. EC is a safe and effective method for preventing unwanted pregnancy and can reduce the risk of pregnancy by up to 99%. In spite of its effectiveness, EC is not frequently used. In many countries, women face barriers to accessing EC. The majority of women in low‑income countries are unaware of EC. Moreover, some providers have negative attitudes toward providing EC to women and girls.
Myth-busting facts about the contraceptive injection
Watch this short animation to learn more about the contraceptive injection, a contraceptive method that requires no daily action and doesn't interfere with sex. Learn more about other methods
TAKING STOCK: IPPF Recommendations on the Global Financing Facility (GFF)
The Global Financing Facility (GFF) is a financing mechanism in support of reproductive, maternal, newborn, child and adolescent health launched in 2015. This IPPF briefing sets out recommendations for GFF stakeholders and financiers as the GFF undergoes its first replenishment process.

The Global Gag Rule: The impact in Burundi
Burundi is landlocked between Democratic Republic of the Congo, Rwanda, and Tanzania. Of the estimated 10.72 million population, 67% live below the poverty line. Association Burundaise pour le Bien-Etre Familial, (ABUBEF) set up in 1991, provides a range of essential services, with a strong focus on HIV. Around 84,000 people are living with HIV in Burundi, of whom 12,000 are children under 14. ABUBEF’s focus is on HIV prevention and management: from youth-friendly counselling to programmes to prevent mother-to-child transmission. The withdrawal of US funding due to the Global Gag Rule will drastically reduce and, in some instances, close ABUBEF’s vital healthcare services and programmes. It is estimated that loss of funding to ABUBEF through the global gag rule will deny 117,016 people access to safe, sexual and reproductive healthcare. ABUBEF currently supports around 2, 123 people with anti-retroviral treatment, who will be affected by the cuts. Donavine Uwimana, Executive Director of ABUBEF, “The GGR affects our very existence, with a forecasted funding cut of 39% in 2017 as well as a major decline in the supply of almost all sexual and reproductive health and HIV commodities.” ABUBEF provides services to a range of clients including people living with HIV such as pregnant women, internally displaced persons and sex workers. The impact through funding losses affects service provision – including safe delivery for HIV-positive women, and a reduction in medical staff and drugs and commodities available. IPPF is trying to find alternative funds to fill the gaps – a combination of long- and short-term measures to avoid closures and reductions in services. Donavine explains how far-reaching the impact is for ABUBEF: “Almost all contraceptives, HIV reagents, STI drugs, antiretroviral and consumables for HIV management are procured through UNFPA, USAID and US-financed government programmes, which will be affected by the GGR,” she says. IPPF visited several ABUBEF run projects at risk of closure across Burundi that included a centre in Kirundo for vulnerable women such as sex workers and survivors of gender-based violence. And in Ngozi, an HIV clinic that provides mobile clinics, and a maternity ward with a focus on the prevention of mother-to-child transmission. Learn more about the Global Gag Rule Help us bridge the funding gap

Putting people first: providing health care despite funding and staff losses in Burundi
The Association Burundaise pour le Bien-Etre Familial's (ABUBEF) provides vital integrated services to local communities, including contraception, prevention and treatment of HIV, youth-friendly counselling and education, pre-marital counselling, and antenatal and post-natal care. ABUBEF has 18 service points, including static and mobile clinics, and community-based services. An estimated 80% of its clients are poor, marginalized, socially excluded and/or under-served. ABUBEF supports young people living with HIV, internally displaced persons, sex workers, drug users and street children. The continuation of many of these vital health services are under threat following the reintroduction of the Global Gag Rule by the US Administration. The Global Gag Rule, or Mexico City Policy as it is formally known, stops US aid to all health programmes run by organisations who perform or counsel on abortion. ABUBEF says: “Almost all contraceptives, HIV reagents, STI drugs, antiretroviral and consumables for HIV management are procured through UNFPA, USAID and US-financed government programmes, which will be affected by the Global Gag Rule.”
Pagination
- Previous page
- Page 7
- Next page






