
The majority of HIV infections are sexually transmitted or are associated with pregnancy, childbirth and breastfeeding.
Our work links prevention with treatment, care and support, reduces HIV-related stigma and discrimination, and responds to unique regional and national characteristics of the epidemic.
Articles about HIV and STIs

Living with HIV - a grandmother's tale
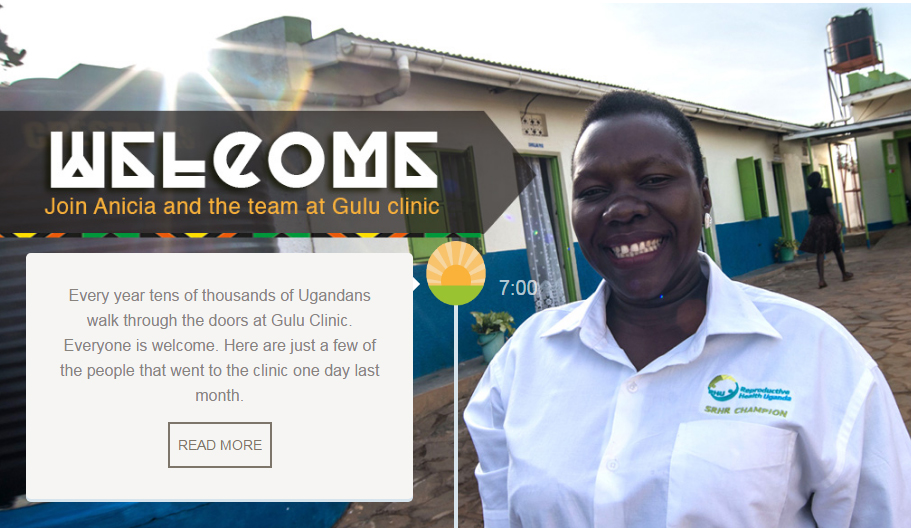
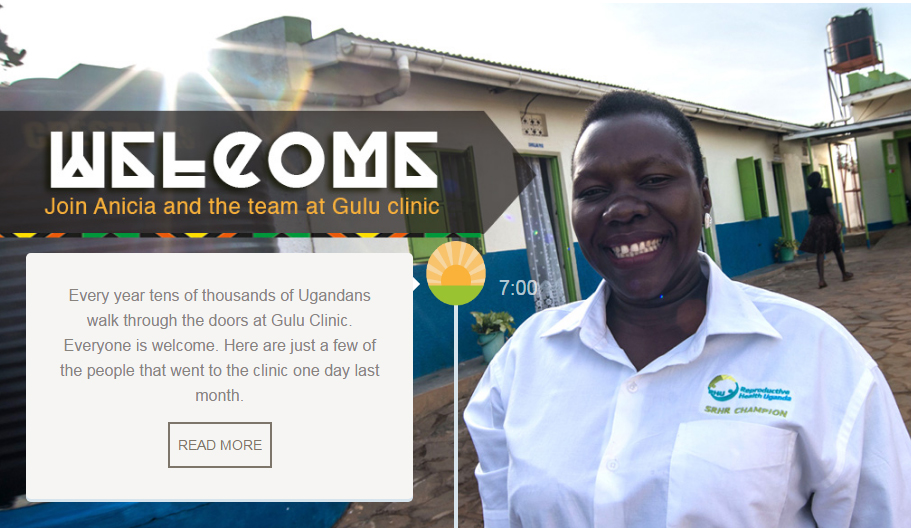
Christine Latim is a 45-year-old grandmother is living with HIV. She has been on antiretroviral treatment since 2005 and was widowed in 2006. She thinks her husband died of an HIV-related infection. “I heard on the radio that for people living positively it was a serious risk for us to get cervical cancer. During the announcements they mentioned some of the signs of cervical cancer like bad smell and so many signs. “I was having signs of discharge and very bad smell,” she said. She needed a smear to check for cervical cancer but getting one in rural Uganda wasn’t easy because money was tight and there were few gynaecologists available. “I tried in TASO Uganda, I failed. I went to Lachor Hospital, I never got satisfied. “Early in 2013, I heard over the radio about the services being offered by Reproductive Health Uganda. I went to their service centre and I was examined for cervical cancer and I tested positive. I got services from that centre. Last August, when I went for my control, they found that I’m free of cervical cancer” said Latim. When she went for the smear for cervical cancer at Gulu Clinic she was also tested for human papilloma virus (HPV). Today Christine is visited by two people at her thatched hut home four kilometres away from Gulu Clinic. It is part of the routine follow-up for patients. From first appearance, it is hard to believe that this grandmother of one is living with HIV until she tells you that she is living positively. In her hut, the portrait of her late husband is displayed on the wall. Smartly dressed in a white and black coloured long dress, Latim said she had seen many friends that had died of cervical cancer. “Gulu Clinic has changed my life completely because of the way they handle their clients. And we got the service at a lower cost than at other health centres. “If I had any capacity to talk to government or any non-governmental body, I would say they should support RHU Uganda for their good service to youth, women and those of us that are positive living” said Latim. Latim’s prayer is that Gulu Clinic scales up more services targeting the youth in her community. “In our country if the youth is healthy many of our youth have experienced a long period of conflict so they need more sensitization especially for their health.” she added. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
Reproductive Health Uganda: A one-stop shop of life-changing services
Reproductive Health Uganda: A one-stop shop of life-changing services" Every year tens of thousands of Ugandans walk through the doors at Gulu Clinic. Everyone is welcome. Here are just a few of the people that went to the clinic one day last month. READ MORE 7:00 "I was suffering…..so my sister decided to bring me here. When she brought me here, I was treated and I got better. I really admired how they do their things and I really wanted to learn more about Reproductive Health." READ MORE 8:00 "I grew up alone. I ended up dropping out of school and I went for sex working. I came purposely here to RHU for Hepatitis B testing and also counselling because I have so many personal problems. I like coming here….they’re so caring." READ MORE 09:00 Fertility treatment remains a sensitive issue for men and women in Uganda but Brenda and her husband, Francis decided to visit Reproductive Health Uganda's clinic in Gulu. “They helped us a lot and we get proper treatment." READ MORE 15:00 "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 16:00 "Our goal is to ensure this Reproductive Health Uganda clinic in Gulu is a 'one-stop-centre'. When a client comes in, she comes out when she has got a very big package of services. And when we go to do outreach in the community we give very many services" READ MORE 17:00 At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am…and we may end up sometimes up to 10pm because we never chase out our client. We’ll never close the place when we have a client inside. People come when they have no hope.” READ MORE 22:00
Living with HIV and HPV - a grandmother's tale
Christine is a 45-year-old grandmother who has HIV. She has been on antiretroviral treatment since 2005 and was widowed in 2006. She thinks her husband died of an HIV-related infection. “I heard on the radio that for people living positively it was a serious risk for us to get cervical cancer. During the announcements they mentioned some of the signs of cervical cancer like bad smell and so many signs. “I was having signs of discharge and very bad smell,” she said. She needed a smear to check for cervical cancer but getting one in rural Uganda wasn’t easy because money was tight and there were few gynaecologists available. “I tried in TASO Uganda, I failed. I went to Lachor Hospital, I never got satisfied. “Early in 2013, I heard over the radio about the services being offered by Reproductive Health Uganda. I went to their service centre and I was examined for cervical cancer and I tested positive. I got services from that centre. Last August, when I went for my control, they found that I’m free of cervical cancer,” said Christine. When she went for the smear for cervical cancer at Gulu Clinic she was also tested for human papilloma virus (HPV). Today Christine is visited by two people at her thatched hut home four kilometres away from Gulu Clinic. It is part of the routine follow-up for patients. From first appearance, it is hard to believe that this grandmother of one is living with HIV until she tells you that she is living positively. In her hut, the portrait of her late husband is displayed on the wall. Smartly dressed in a white and black coloured long dress, Christine said she had seen many friends that had died of cervical cancer. “Gulu Clinic has changed my life completely because of the way they handle their clients. And we got the service at a lower cost than at other health centres." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

Youth volunteers leading the change in Uganda
Nancy Lakisa, a 19-year-old nursing student, volunteers at Reproductive Health Uganda Gulu branch. Nancy first went to the clinic as a client when she was suffering from a burning urinary tract infection. RHU clinics offer integrated youth-friendly services to encourage young people to use health services and staff have been trained to listen and offer services to adolescents with ease and respect. “When I came for the service, I was welcomed, I felt at home because the service provider handled me in a very good way. Though I was afraid of telling her what was happening to me but the way she was talking to me, I really got that courage and explained to her everything. "I am inspired to be a caring nurse and now I spend my holiday time at the clinic as a volunteer. I really admired how they do their things and I really wanted to learn more about reproductive health." Nancy said her experience had changed her life. “I had many boyfriends, I used not even to care whether somebody talked me. I didn't even used to respect my mum when she tried to advise me but I had counselling about that. I only have one life. Gulu is changing the lives of many people." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

Putting clients first: a one-stop shop of outreach services in Gulu, Uganda
.p { text-align: justify; align: left; } Uganda has one of the highest fertility rates in the world, and as a result, it also has one of the most youthful populations - more than half of Ugandans are under the age of 15. Over 78% of the population is below the age of 30. The population is growing at a rate of more than 3% per year. Figures show that women – on average - give birth to two more children than they want. More than half of pregnancies in Uganda are unintended, and nearly a third of these end in abortion according to figures from the Guttmacher Institute. It also says that in Uganda approximately one in every 19 women has an abortion per year and with abortion being highly restricted most of these are unsafe. This rate is far higher than the average for East Africa and reflects the high level of unmet need for contraception in the country. Approximately, 755,000 unintended pregnancies occur annually out of which 297,000 result in unsafe abortions. Unintended pregnancy is common in Uganda, leading to high levels of unplanned births, unsafe abortions, and maternal injury and death. Women in the eastern and north regions had the highest proportions of unplanned births (50–54%) the high levels of unintended pregnancy and unplanned births in Uganda can be attributed primarily to nonuse of contraceptives by women who do not want a child soon. More than 80% of the population lives in rural areas. Millions of people still do not have access to a health clinic, and family planning, especially long term and permanent methods, is not available to the vast majority who live in rural and hard-to-reach areas. IPPF’s Member Association, Reproductive Health Uganda (RHU), is working hard on the ground to tackle these issues. It takes the approach that it offers people as many services as possible at its clinics so you can get your health needs met in the same place. This means you might go to a clinic for an HIV test but leave having being offered a range of contraception plus other tests for other sexually transmitted diseases or cancer. RHU has a network of clinics across the country and takes its services out to remote and rural areas through its mobile clinics. No one is left out by RHU. Whether people are poor or vulnerable or hard to reach, RHU makes sure they have access to all of the services they need. We visited one of RHU’s health facilities in northern Uganda to get a better idea of how our work makes a real difference to people and their lives. We wanted to hear stories about what difference getting contraception, counselling and testing meant in reality. For many people it is life-changing. Thousands of people go in and out of Gulu Clinic every year and thousands more get services through Gulu’s mobile clinics. Last year alone Gulu Clinic had 229,812 family planning clients and provided 769,707 sexual health services, 390,488 of those were to young people. It offers a ‘one-stop-shop’ approach which makes it easier for clients to get a range of integrated services. They can go to a clinic for a check-up but end up getting contraception, counselling and a whole range of other tests and treatments. These include family planning, infertility management, cervical cancer screening, cryotherapy, youth friendly services, sexually transmitted infections and general sexual and reproductive health (SRH). Denis Bongonyinge, who has worked at Gulu Clinic for four years, said: “For us our goal is to ensure that this place is just a one stop centre. When a client comes in, he goes out when he has got a very big package of services within the clinic. Even if we go out, we give very many services. Denis said he had come across a range of issues among the clients. Issues like high rates of teenage pregnancies, sexually transmitted infections and gender based violence which could all be dealt with at the centre. He added that he believed Gulu had managed to offer such a range of services because of its willingness to work with other partners interested in scaling up uptake of family planning and generally sexual and reproductive health services. Gulu Clinic is also inclusive to a wide range of people across the community and this includes sex workers and disabled people. Vicky Acora is deaf and has had problems getting services at other hospitals. But, she says about RHU: “They are really most welcoming and they try to communicate even in the little sign language they know. They are really very warm” She says she has since been advising other deaf persons to seek services at Reproductive Health Uganda because of the quick services. “I encourage other people to come here because it is fairer. I encourage other disabled people who use wheelchairs not only the deaf to come and access services here because it is really accessible for those who have a disability.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
Changing lives in Nigeria
Nigeria has Africa’s biggest population. And it’s still growing at 3% a year. A lack of family planning is one reason – many women and girls want contraception – but like millions around the world – can’t get it. But that could be about to change, thanks to a pilot project run by Planned Parenthood Federation of Nigeria (PPFN), IPPF’s national member. It’s proving a huge success. This is its story, told by the women whose lives it has changed and the people working to change them. LAUNCH THE INTERACTIVE STORY
Gulu clinic: A one stop shop of services in rural Uganda
Uganda has one of the highest fertility rates in the world, and as a result, it also has one of the most youthful populations - more than half of Ugandans are under the age of 15. Approximately, 755,000 unintended pregnancies occur annually out of which 297,000 result in unsafe abortions. We are working hard on the ground to tackle these issues. Our Member takes the approach of offering people as many services as possible to get all health needs met in the same place. See a day in the life of the staff and clients of Gulu clinic, Uganda.

Is the 2016 Political Declaration on Ending AIDS finally a ‘farewell to abstinence and fidelity’?
Mikaela Hildebrand,Senior Policy Adviser - for Sexual and reproductive health and rights, from IPPF's Swedish Member Association writes a short reflection on the High Level Meeting on AIDS, published in the Lancet this week. Negotiators at #UN choose evidence over ignorance: choose #sexed over#abstinence in #AIDS Declaration https://t.co/cHEEyxOZw9 — RFSU (@RFSU) August 16, 2016 "In June 2016 I took part in the 2016 United Nations General Assembly High Level Meeting on AIDS as part of the Swedish Delegation. As RFSU, the Swedish Association for Sexuality Education and IPPF MA, together with many other committed organisations, we had followed the negotiations for a good few months. We had focused our advocacy on comprehensive sexuality education, and we knew the oppositions would be tough. We needed a political declaration that delivered a policy commitment to evidence informed programmes to advance comprehensive sexual and reproductive health and rights, comprehensive sexuality education included, to re-shape HIV prevention efforts. Much was at stake. Comprehensive knowledge about correct and consistent HIV prevention remains appallingly low, and has stalled over the past 15 years. New HIV infections have only dropped about 8% from 2010 to 2014 among young people and adults, and there still are some 2000 new HIV infections among young people every day. While the assessment of the outcome document has been rather polarized with some seeing it as a failure while others hail it as a great success, when it comes to comprehensive sexuality education, the outcome document all but mentions the concept. Paragraph 62 (c) reads: Commit to accelerate efforts to scale up scientifically accurate age- appropriate comprehensive education, relevant to cultural contexts, that provides adolescent girls and boys and young women and men, in and out of school, consistent with their evolving capacities, with information on sexual and reproductive health and HIV prevention, gender equality and women’s empowerment, human rights, physical, psychological and pubertal development and power in relationships between women and men, to enable them to build self- esteem, informed decision-making, communication and risk reduction skills and develop respectful relationships, in full partnership with young persons, parents, legal guardians, caregivers, educators and health-care providers, in order to enable them to protect themselves from HIV infection; While the word sexualty is missing, all the core elements of comprehensive sexuality education are there. However the most important thing, are the two missing words: abstinence and fidelity. This small omission, is infact a hard won major gain from the negotiations and signals a much needed shift in HIV prevention from dogma to evidence. On the last day of the meeting, when the negotiations had been sealed and the Political Declaration adopted, I had a conversation with Kent Buse, chief of Strategy and Policy Directions at UNAIDS on the the importance of these missing words. We decided it needed highlighting. So together with Sarah Hawkes, Professor at University College London, we wrote a commentary that was published today in the Lancet Global Health, to make sure that the removal of these two concepts from the toolbox of HIV prevention, at least at a global policy level, does not go unnoticed. Now we need to translate this policy commitment to action through follow up at country level and challenge outdated national frameworks. The commentary outlines the following four point policy action agenda: Update country policy frameworks and abandon abstinence-based and fidelity-based HIV prevention programmes, in consultation with technical agencies Develop comprehensive sexuality education curricula that include addressing gender-power dynamics to deliver on the sexual health and gender equality targets of the 2030 Agenda for Sustainable Development, and strengthen capacity of teachers to deliver it Work with teachers' unions, parent associations, and traditional and community leaders to shift community perspectives on comprehensive sexuality education and the delivery of comprehensive sexual and reproductive health programmes in and out of schools Support advocates, including youth groups, to hold their governments accountable for international commitments made, including in the Political Declaration on HIV and AIDS" You can read the full commentary here: http://www.thelancet.com/journals/langlo/article/PIIS2214-109X(16)30138-3/fulltext

IPPF and Durex join forces to raise awareness of Zika as an STI
Global #DontShareZika campaign launched to spread the message with an educational video and condom giveaway. As the global focus shifts to Brazil, the world’s leading sexual wellbeing brand Durex and the International Planned Parenthood Federation (IPPF) have joined forces to launch #DontShareZika, a global campaign to raise awareness of the Zika virus, educate about its status as a sexually transmitted infection (STI) and provide direct support by handing out millions of free condoms. We're working with @ippf to help stop the spread of #Zika. Want to help? Share this, but #DontShareZika… pic.twitter.com/hdhx51sEi2 — Durex Global (@durex) August 5, 2016 The move follows the update by the World Health Organization (WHO), confirming that in addition to being spread by infected mosquitoes, Zika* can also be transmitted sexually. This means that everyone - including people in a monogamous relationship - may be at risk from the STI if they, or their partner, have visited an affected area and been bitten by an infected mosquito. As an STI, the Zika virus has the potential to travel and spread between people who may not even realise they are infected. In response, Durex have created the #DontShareZika video to educate that the Zika virus can be passed between couples during unprotected sex, and committed to a giveaway of three million free condoms in Brazil. WHO recommends that men and women returning from an area where Zika is circulating should practice safer sex, including through the correct and consistent use of condoms, for at least eight weeks after leaving an affected area, even if they don’t have symptoms. At a time when Brazil is expecting as many as a million extra visitors from across the globe, the #DontShareZika campaign aims to spread this important message as widely as possible to limit the risk of further infections. #DontShareZika follows recent work by Durex lobbying for the world’s first safe sex emoji** designed to help young people discuss safe sex. Both initiatives are part of Durex’s continuous efforts for better sexual health and education globally. “As the world’s number one sexual wellbeing brand we have a responsibility to make people aware of this STI, to help people to stay healthy and to prevent the sexual transmission of the virus.” commented the Global Director ofRB the brand, Volker Sydow. IPPF Director General Tewodros Melesse, added; “Our aim is to ensure all people have access to sexual and reproductive health information and services. At the moment, many people still don’t realise that Zika can be transmitted sexually. Communicating this and enabling people to protect themselves and their partners is critical, so we welcome #DontShareZika and Durex’s free condom giveaway in Brazil.” Durex are calling for people to support the campaign and help share a message of protection and prevention faster than this STI, Zika, can be spread, by sharing the informative video and using the hashtag #DontShareZika. Follow @Durex for more information. For more information on the Zika virus visit: http://www.who.int/mediacentre/factsheets/zika/en/. -ENDS- For further information please contact Amy Williams: [email protected]/ 0207 292 5084 or Toby Leston: [email protected]/ 0207 2929 6451 Notes to Editors * Zika virus is linked to microcephaly - a condition where babies are born with brain damage and undeveloped heads. ** www.youtube.com/watch?v=O7iKgKpkWfU About Durex Durex® is the #1 sexual wellbeing brand worldwide. The brand not only produces condoms that exceeds global testing standards, but also offers pleasure gels, lubricants and personal massagers. With over 80 years of experience in the bedroom, Durex is dedicated to inspiring lovers to love sex safely. That is why Durex will never stop innovating with new products that enhance the sexual experience, helping couples get closer and go further together. For more information, go to www.Durex.com. About RB* RB is the world’s leading consumer health and hygiene company. The company has operations in over 60 countries, with headquarters in London, Dubai and Amsterdam, and sales in most countries across the globe. The company employs approximately c. 37,000 people worldwide. Inspired by a purpose to deliver innovative solutions for healthier lives and happier homes, RB is in the top 20 companies listed on the London Stock Exchange. We are the global No 1or No 2 in the majority of our fast-growing categories, driven by an exceptional focus on innovation. Our health, hygiene and home portfolio is led by our global Powerbrands including Nurofen, Strepsils Gaviscon, Mucinex, Durex, Scholl, Clearasil, Lysol, Dettol, Veet, Harpic, Cillit Bang, Mortein, Finish, Vanish, Calgon, Air Wick, Woolite and French’s. Our Powerbrands represent 80% of net revenue. RB is redefining the world of consumer health and hygiene. Our people and unique culture are at the heart of our success. We have a drive for achievement and a passion to outperform wherever we focus, including sustainability where we are targeting a 1/3 reduction in water impact, 1/3 reduction in carbon and 1/3 of net revenue from more sustainable products. We are proud to be Save the Children’s largest global partner, with a new vision to radically reduce one the world’s largest killer of under 5s, diarrhea. For more information visit www.rb.com. *RB is the trading name of Reckitt Benckiser group of companies About IPPF IPPF delivers sexual and reproductive health services that let people make their own choices. We fight for everyone to have the right to make those choices. We are local, through our members and volunteers, and global, through our network. We meet need, wherever it is, whoever requires it, for as long as they want it.

Ending HIV infections among young women – making men part of the solution
by Jon Hopkins, IPPF Senior HIV Officer Whilst at the 2016 International AIDS Conference –held in Durban from 18-22nd July 2016 – I heard repeatedly that whilst huge progress has been made in addressing HIV since the last AIDS Conference in Durban in 2000 – one of the areas that needs urgent attention is stopping new HIV infections among adolescent girls. Every week over 1000 young women aged 15-24 acquire HIV, two-thirds of them live in sub-Saharan Africa. This is both due to a lack of knowledge about sexual health and gender inequalities, including gender-based violence, that exacerbate young women’s vulnerability to HIV and blocking their access to HIV services. The standard response in addressing the high level of HIV acquisition among young women is typically to position men as “the problem”. Men are seen as the cause of HIV among young girls – they are promiscuous, they refuse to use condoms, they are the perpetrators of violence and so on. The response therefore is to focus on empowering women and enhancing their abilities to protect themselves, with less attention devoted to engaging men to curb their own HIV risk, to reduce the risk their behaviours may pose to others and to access services that can protect their health and lives. This not only reinforces the assumption that HIV prevention falls within the domain of women’s lives and “duties”, it also risks estranging men who might otherwise be open to becoming more engaged in their own and their partners’ health. The latest HIV data from UNAIDS show that a man is less likely than a woman to take an HIV test, and to seek, use and adhere to HIV treatment. When men living with HIV are ignorant of their HIV-positive status, it lengthens the time that they put their sexual partners at risk of HIV infection. It also delays their own treatment and care, and puts their lives at risk. In sub-Saharan Africa, where men 40% of people living with HIV were men, they accounted for 54% of all deaths. These data are shocking – but what does this have to do with adolescent girls and young women? Africa Centre survey data from South Africa describes a cycle of HIV transmission. In the populations studied, women in their teens and early 20s tended to acquire HIV from men older than 25 years, many of who were recently infected and had high viral loads. Once those young women reached and passed their mid-20s, some transmitted HIV to their male peers, some of who then continued the cycle of transmission to younger women and adolescent girls. Data from Swaziland shows a very similar pattern with young women (aged 16-23) acquiring HIV from a man an average of eight years older. Protecting women in their teens and early 20s from acquiring HIV therefore also requires preventing HIV acquisition in men who are in their mid-20s and older – and vice versa. This requires an inclusive approach which reduces HIV risk for everyone. But what does this inclusive approach look like? At the AIDS Conference, a Platform for Action – developed following a High Level Consultation convened by UNAIDS, Sonke Gender Justice and IPPF – was launched, which highlight four key actions which are required in order to overcome the “blind spot” to men which exists in the current HIV response. First is the need to better understand what is happening by generating and using disaggregated data on men’s access to and use of HIV-related services and solid analysis and use of this data at the local level for decision making. Second is realising that existing HIV services are not sufficiently reaching men and men are not engaging with the available HIV services – especially in sub-Saharan Africa. When men do not have access to services, this is harmful to them, harmful to their partners and harmful to their families. Therefore it is critical that policies include more focus on reaching men and adolescent boys with innovative service delivery methods in workplaces, places of worship, sports gatherings and other community venues. Crucially, any efforts to improve health service access for men and boys should not come at the expense of women and girls’ access and rights. Thirdly, practical improvements in the design and delivery of services need to occur against a backdrop of efforts to challenge gender privileges that accrue to men and boys. Rather than seeing men purely as the problem, they should be constructively engaged as “agents of change” whilst changing the negative powerful notions of “manhood” and masculinity to positive ones that encourage health seeking behaviour, increasing men’s role as a supportive partner, and addressing the underlying factors that lead men to be violent towards their partner. Finally, sustaining these actions requires supportive legal frameworks and strategic alliances, along with adequate technical and financial resources for assessing, strengthening and expanding actions. Greater support for community systems and networks is also vital. If the goal to ‘end AIDS by 2030’ is going to have any chance of success, HIV programmes also need to include specific programmes that support HIV prevention, testing, treatment and adherence among men and adolescent boys. Done correctly – in a way that builds upon and enhances efforts focused around the health of women and girls – this will improve the health of men, the health of their partners, and the health of their families. Therefore, to prevent HIV in young women, we need to transform HIV programmes to make men part of the solution, not just part of the problem.
Pagination
- Previous page
- Page 11
- Next page






