
The majority of HIV infections are sexually transmitted or are associated with pregnancy, childbirth and breastfeeding.
Our work links prevention with treatment, care and support, reduces HIV-related stigma and discrimination, and responds to unique regional and national characteristics of the epidemic.
Articles about HIV and STIs
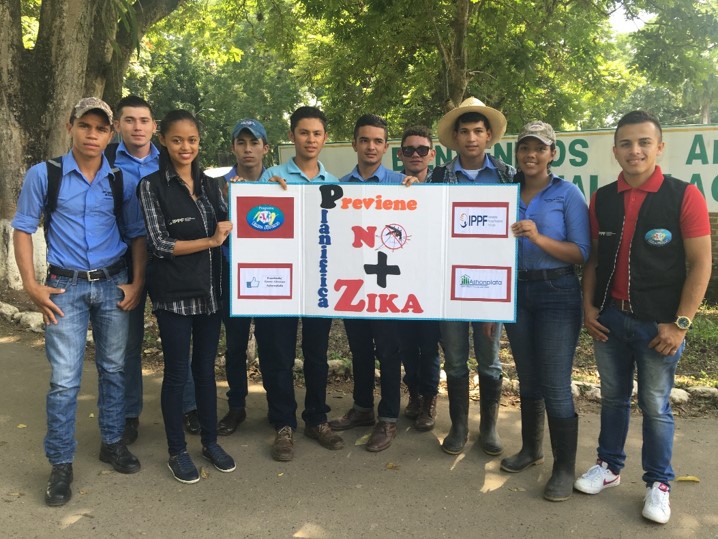
SIFPO 2: Supporting voluntary family planning and Zika prevention in countries affected by Zika
The rapid spread of the Zika virus by mosquitos and through sexual contact, prompted the World Health Organization to declare a public health emergency in 2016. Women living in Caribbean and South American favelas and in rural areas, where mosquitos are a part of everyday life and where sanitation is poor, are more susceptible to infection and less likely to have access to sexuality education, and family planning services. Government recommendations to delay pregnancy cannot be realized without improved access to voluntary family planning. Zika presents a new challenge to health workers in South and Central America as the outbreak of Zika has led to an increase in demand for voluntary family planning services amongst women of reproductive age who are at risk of or affected by Zika. Although information about Zika has made the headlines around the world, women in countries affected by Zika often lack information about the virus. In particular, information is sparse about the sexual transmission of Zika, and how family planning can be used to reduce risk of infection and avoid unplanned pregnancies. Providers have not been trained before on how to screen women for Zika, or support couples to make important decisions about family planning in the context of the outbreak. In response to the Zika outbreak, IPPF is helping its network of clinics and community and mobile health programmes to increase access to contraceptives and broaden public awareness about the virus. This work will be carried out in close collaboration with national governments and other health providers to ensure maximum impact and avoid duplication of efforts. The USAID funded SIFPO2 project is supporting 4 MAs in Honduras, the Dominican Republic, Guatemala and El Salvador to scale-up out-reach services in high burden areas; training government health workers on Zika and family planning counselling; and integrating Zika information into contraceptive counselling and antenatal care across IPPF’s extensive network of clinics. The objectives of the activity are: To improve women of reproductive age’s access to healthcare services in Zika-affected or at-risk communities to promote informed and safe conception, including antenatal and postnatal care, child development and FP services. To improve providers’ capacity to deliver high quality Zika-related healthcare and social services to women of reproductive age, specifically pregnant women, families and children affected by Zika. Results to date: 1,000 health workers received specialist training in 2016 in Zika prevention and voluntary FP services. Providers have been given guidance and protocols on how to counsel non-pregnant women on Zika prevention, and on screening and counselling for pregnant women during routine antenatal check-ups. In 2017, the project plans to reach hundreds more providers. Each of these health care workers will go on to deliver high quality Zika-related healthcare to women, couples and families at a time when they need it most. The project is supporting an expanded network of voluntary FP services through mobile clinics and via community workers to ensure access in the poorest and hardest to reach areas In Honduras, IPPF’s Member Association is the only organisation working to educate and inform the public about sexual transmission of the Zika virus In El Salvador, IPPF’s Member Association is facilitating radio messages to share information about Zika. In Guatemala, community-based promotors reached nearly 1,500 people with Zika prevention messaging in December alone. This information enables women and families in poor communities to make informed decisions about how to protect their health and their futures. The Support for International Family Planning Organizations 2 – Sustainable Networks project is a five-year cooperative agreement funded by the U.S. Agency for International Development under Agreement No. AID-OAA-A-14-00038, beginning May 13, 2014. The information provided in this document is not official U.S. government information and does not necessarily represent the views or positions of the U.S. Agency for International Development.

‘Hands Up for HIV Prevention’ says IPPF Director General in Swaziland for World AIDS Day 2016
Mankayane, Swaziland - On 1 December, IPPF Director General, Tewodros Melesse, made an address on the occasion of World AIDS Day in the Kingdom of Swaziland along with His Excellency the Right Honourable Deputy Prime Minister, Mr Paul Dlamini, Honourable Minister of Health Ms Sibongile Ndlela Simelane, United Nations Resident Coordinator, Mr Israel Dessalegne, and the United States of America Ambassador to Swaziland, Ms Lisa Peterson. "It is an honour and a privilege to be commemorating World AIDS Day with you, the Swazi people. Every year, World AIDS Day provides us with the opportunity to take stock of how far we have come since the early days of the epidemic. I’d like to begin by taking us 30 years back in time, which was 1986. That year, IBM unveiled the first laptop. Mobile phones were the size and weight of large bricks. In apartheid-era of South Africa, Nelson Mandela was behind bars; and here in Swaziland, the country recorded its first case of HIV/AIDS. Many of you here today will agree with me when I say that, while Swaziland has not been immune to the many ways in which the world has changed over the past thirty years, it is the HIV epidemic more than anything else that has shaped this country during that time. For those of you who have lived through the epidemic, you will remember all too well the fear and the stigma that ran through this country and many African countries. You will remember how little we knew about HIV, and about how to prevent it. People living with HIV at this time deserve to be honoured. You showed us the strength and determination to fight for change. You were brave and angry, and gave hope to others. As I stand in front of you, I am keenly aware that there is not a single person here whose life, one way or another, has not been affected by HIV, and that all young people here today have never seen a world without HIV. The young people are the future but we have to remind ourselves that there is no future if we don’t invest in prevention. Many of you have loved ones who were taken from this world before their time. You grieved and continue to grieve the loss of brothers, sisters, mothers, fathers, children, grandchildren, friends, colleagues, and many others. These vibrant souls, remain with us always, in our hearts and in our minds, and give us energy to continue in the future. We can now take some comfort from the fact that the picture has changed dramatically in these past thirty years. Most significantly, people living with HIV are now living longer, healthier, and productive lives well into their old age, thanks to the availability of antiretroviral treatment that has transformed HIV infection into a chronic, manageable condition. I would like to take this moment to commend the Government of the Kingdom of Swaziland for its commitment to providing antiretrovirals free to all who need treatment. The impact of this cannot be underestimated. AIDS-related mortality has reduced by drastically and accordingly, life expectancy has now rebounded. The transmission of HIV from mother to child is close to being eliminated along with syphilis. And overall, Swaziland has also begun to see a downward trend of new HIV infections, especially among young people. ‘Now is not the time to be complacent’ These are remarkable successes, and Swaziland has established a strong foundation. Critically, this is a foundation upon which to build - not to rest. We cannot risk becoming complacent, as HIV remains the greatest public health and socio-economic challenge facing this country. Importantly, our response must be integrated with other key challenges. We know that there is a high unmet need for family planning, leading to high levels of unwanted pregnancy; we know that maternal and infant mortality is unacceptably high; and we know that the overall knowledge of sexual and reproductive health is exceptionally low among young people. ‘There is a serious prevention gap’ This situation is not unique to Swaziland. UNAIDS is raising the alarm about the global picture and what it calls the ‘prevention gap’. Efforts to meet the global target of ending AIDS by 2030 are off track and progress is at risk of stalling. The global community warns that if there is a resurgence of HIV, the epidemic will be impossible to control. This cannot be allowed to happen. Primary prevention has been and will continue to be an essential component of the HIV response. To attain an AIDS-free generation, we need new solutions, new innovations and, importantly, we need to reinvigorate our prevention efforts. Prevention saves lives, saves budget, and increases productivity. ‘Hands Up for HIV Prevention’ Today, people across the global are raising their hands to HIV prevention this World AIDS Day. There is no ‘one size that fits all’ and we must pay special attention to those that continue to be left behind. Young women and girls are at a particularly high risk of HIV infection. They need information and the freedom to make free and informed decisions about their sexual and reproductive health; they need access to effective HIV and sexual and reproductive health services; they need services that are youth-friendly; and they need gender-based violence to be eliminated and gender inequalities to be eradicated. We are also leaving key populations behind – including sex workers, people who inject drugs, transgender people, and men who have sex with men. Many countries in the world push these populations to the margins of society. It is essential that our prevention efforts bring these populations forward. To end HIV, no one can be left behind. I must commend the efforts to ensure the meaningful engagement of these populations; and by taking steps to remove barriers to access services. At the root of all of our prevention efforts is a recognition that the HIV epidemic is being fuelled by inequalities and prejudices entrenched within the legal, social and economic structures of society. Poverty, sexism, homophobia, and other forms of discrimination – are well known barriers to ending HIV. To ensure that everyone can live a life of hope, with dignity, respect and meaning – people must be free to make choices about their sexuality and well-being, in a world without discrimination. ‘We need to work together to give hope’ I truly believe that we will not see an end to HIV unless we work together, be it at the local level, the regional level or at the global level. The remarkable successes that we have witnessed have been the result, not of a single actor, but of a chorus of voices that have called out in unison for better access; and that demanded respect, care and compassion. Civil society in particular has an incredible track record of mobilizing the required response. It has been instrumental in changing public attitudes and perceptions, and has also be mobilised to address barriers that prevent people from realising their right to health. In conclusion, the power to end HIV and AIDS does not lie with a single individual, with a single organisation, or government structure. When we leverage the unique skills that we all bring to the table, we will reach our goal of ending AIDS both in Swaziland and the world. This power is ours and the time to act is now. If we work together as Obama says, ‘Yes, we can!’, then we can do it. I leave you with a story. Like FLAS, I visited the IPPF association in Iran who are working with underserved communities, such as sex workers, and integrating in society. I asked one young woman, ‘if you were God for fifteen minutes, what would you do?’ She said, ‘I would give hope, if you have hope, you can overcome your challenges’. We need to keep that hope and give that hope to the people. We can give that hope by doing it together."

Young people must be at the forefront of HIV prevention
This year to mark World AIDS Day I travelled to Swaziland in southern Africa. I saw and heard first hand stories from a country that has made huge inroads in its efforts to curtail the HIV epidemic but it also led me take stock. The @ippf Director General with the Minister of Health and Dudu Simelane former Executive Director at FLAS, now with @IPPFAR #WorldAIDSDay pic.twitter.com/1xkvEkp3tT— FLAS | Temndeni (@FLAS79) December 1, 2016 It made me think about the 78 million people who have become infected with HIV and remember the 35 million who have died from AIDS-related illnesses. Great progress has been made in dealing with the HIV epidemic, especially with the increasing number of people living with HIV on treatment but we cannot become complacent as the decline in new HIV infections among adults has stalled. Globally, critical attention needs to be paid to reinvigorate HIV prevention efforts, with young people at the front and centre of the response. World AIDS Day is a good day for us to reflect and re-state our commitments to end the AIDS epidemic by 2030 as part of the Sustainable Development Goals. At the International Planned Parenthood Federation (IPPF) we remain committed to an integrated HIV and sexual and reproductive health (SRH) response. Of particular importance are young women and adolescent girls. According to UNAIDS nearly 7500 young women aged 15-24 years acquired HIV every week in 2015, the vast majority in southern Africa. In Swaziland, the HIV prevalence among young women aged 15-19 years is 10 per cent compared with 2 per cent among young men of the same age. The transition to adulthood is a particularly challenging time for girls in sub-Saharan Africa, who face a high risk of HIV infection and other sexually transmitted infections, unwanted pregnancies, and violence. This heightened vulnerability is intricately linked to deeply entrenched gender inequalities, harmful gender norms, and structures that limit women and girls from reaching their full potential. Young people within key populations also face particular HIV risks, including young men who have sex with men, young people who sell sex, young transgender people, and young people who inject drugs. This is often due to lower knowledge of risks or lower ability to mitigate those risks compared with their older, more experienced counterparts. These young people are often more vulnerable to discrimination, bullying, harassment, family disapproval, social isolation and violence. Also, young key populations often represent overlapping vulnerabilities and cannot be seen in discrete boxes, requiring a response that recognizes young people in all their diversity. This time last year, IPPF signed a memorandum of understanding with UNAIDS to ‘Fast-Track’ access to HIV prevention, testing and treatment options and SRH services by 2020. Under this partnership, IPPF is committed to deliver concrete actions to reach the most underserved people and ensure young people have the knowledge and means to protect themselves from HIV. Within IPPF’s Strategic Framework 2016-2022, we have committed to deliver 1.5 billion rights-based SRH services, including HIV, and reach 500 million young people with quality comprehensive sexuality education (CSE) programmes. The power to end HIV does not lie with a single individual, with a single organization, or government actor. When we leverage the unique skills that we all bring to the table, we will reach our goal of ending AIDS both in Swaziland and the world. This power is ours and the time to act is now. Director General of the @ippf joining the #handsupforhivprevention campaign in #Swaziland during the #WorldAIDSDay commemoration. pic.twitter.com/aYTTK1WK8G— FLAS | Temndeni (@FLAS79) December 1, 2016
IPPF & Durex launch World AIDS Day Campaign video
IPPF join forces with Durex on December 1st to raise awareness of the risks of unprotected sex as more than 75% of 16-35 year olds surveyed* use emojis to discuss sex, with 9 out of 10 claiming that a safe sex emoji would help them to talk more openly about safe sex. * 3GEM research questioning 3500 people from UK, USA, Brazil, China, India and South Africa commissioned by Durex – UK, October 2016

IPPF joins Durex on World AIDS Day to detail the risks of unprotected sex
“Open Umbrella with Raindrops” emoji revealed as the people’s choice following a global poll* in response to Unicode’s refusal to create an official Condom Emoji. To mark World AIDS Day Durex calls for people to use and share the “Umbrella with Raindrops” emoji to help raise awareness of the risks associated with unprotected sex More than 75% of 16-35 year olds surveyed1 use emojis to discuss sex, with 9 out of 10 claiming that a safe sex emoji would help them to talk more openly about safe sex Almost 50% of 16-35 year olds think that HIV is not something that could ever affect them** despite the fact that every 30 seconds a young person is infected with the virus*** As part of Durex’s ongoing #CondomEmoji campaign, the World’s leading sexual wellbeing brand has today announced “Umbrella with Raindrops” as the overwhelmingly preferred choice in a global poll* to name the unofficial safe sex emoji. To mark World AIDS Day on December 1st, Durex is calling for people across the globe to use and share the emoji in order to raise awareness of the risks associated with unprotected sex and to demonstrate to Unicode the need for an official #CondomEmoji to be approved and appear on every smartphone. The campaign was launched following the shocking revelation that almost half of 16-35 year olds surveyed felt that HIV is not something that could ever affect them despite the reality that every 30 seconds a young person is infected with HIV***. More than 60% of young people surveyed* admitted to being uncomfortable discussing safe sex, with 72% of respondants admitting they found it easier to express emotions using emojis and more than three quarters admitted that they used emojis to discuss sex and relationships. When questioned 9 out of 10 agreed that an official #CondomEmoji would be something that would help them to talk more openly about safe sex. Durex Global Category Director, Volker Sydow, said: “At Durex we believe that for this World AIDS Day identifying the unofficial safe sex emoji is an important step that helps to empower young people to put safe sex back on the agenda, supporting the fight to reduce the spread of HIV and AIDS. We are asking people to show their support for the cause by using this unofficial safe sex emoji and sharing the hashtag #CondomEmoji.” The campaign has also received the support of the International Planned Parenthood Association (IPPF), with Director General Tewodros Melesse adding: “Safe sex awareness continues to be an important global challenge. We support Durex’s campaign in helping make young people think about protection. On World AIDS Day we will be backing this effort to help raise awarness of the risks associated with unprotected sex.” Durex have created an online video as part of the campaign: Sources: * 3GEM research questioning 3500 people from UK, USA, Brazil, China, India and South Africa commissioned by Durex – UK, October 2016 ** Someone Like Me, VIMN & Brand Solutions Insight with Tapestry Research, 2014 *** UNAIDS. Global Report 2010, Core Slides, Slide 11 About Durex Durex® is the #1 sexual wellbeing brand worldwide, producing a wide range of products, including high quality condoms, intimate lubricants and personal massagers. With over 80 years of experience in the bedroom, Durex is dedicated to inspiring lovers to love sex safely. That is why Durex will never stop innovating with new products that enhance the sexual experience, helping couples get closer and go further together. For more information, go to www.Durex.com. About RB* RB* is the world’s leading consumer health and hygiene company. The company has operations in over 60 countries, with headquarters in London, Dubai and Amsterdam, and sales in most countries across the globe. The company employs approximately c. 37,000 people worldwide. Inspired by a purpose to deliver innovative solutions for healthier lives and happier homes, RB is in the top 20 companies listed on the London Stock Exchange. We are the global No 1or No 2 in the majority of our fast-growing categories, driven by an exceptional focus on innovation. Our health, hygiene and home portfolio is led by our global Powerbrands including Nurofen, Strepsils Gaviscon, Mucinex, Durex, Scholl, Clearasil, Lysol, Dettol, Veet, Harpic, Cillit Bang, Mortein, Finish, Vanish, Calgon, Air Wick, Woolite and French’s. Our Powerbrands represent 80% of net revenue. RB is redefining the world of consumer health and hygiene. Our people and unique culture are at the heart of our success. We have a drive for achievement and a passion to outperform wherever we focus, including sustainability where we are targeting a 1/3 reduction in water impact, 1/3 reduction in carbon and 1/3 of net revenue from more sustainable products. We are proud to be Save the Children’s largest global partner, with a new vision to radically reduce one the world’s largest killer of under 5s, diarrhoea. For more information visit www.rb.com. *RB is the trading name of Reckitt Benckiser group of companies
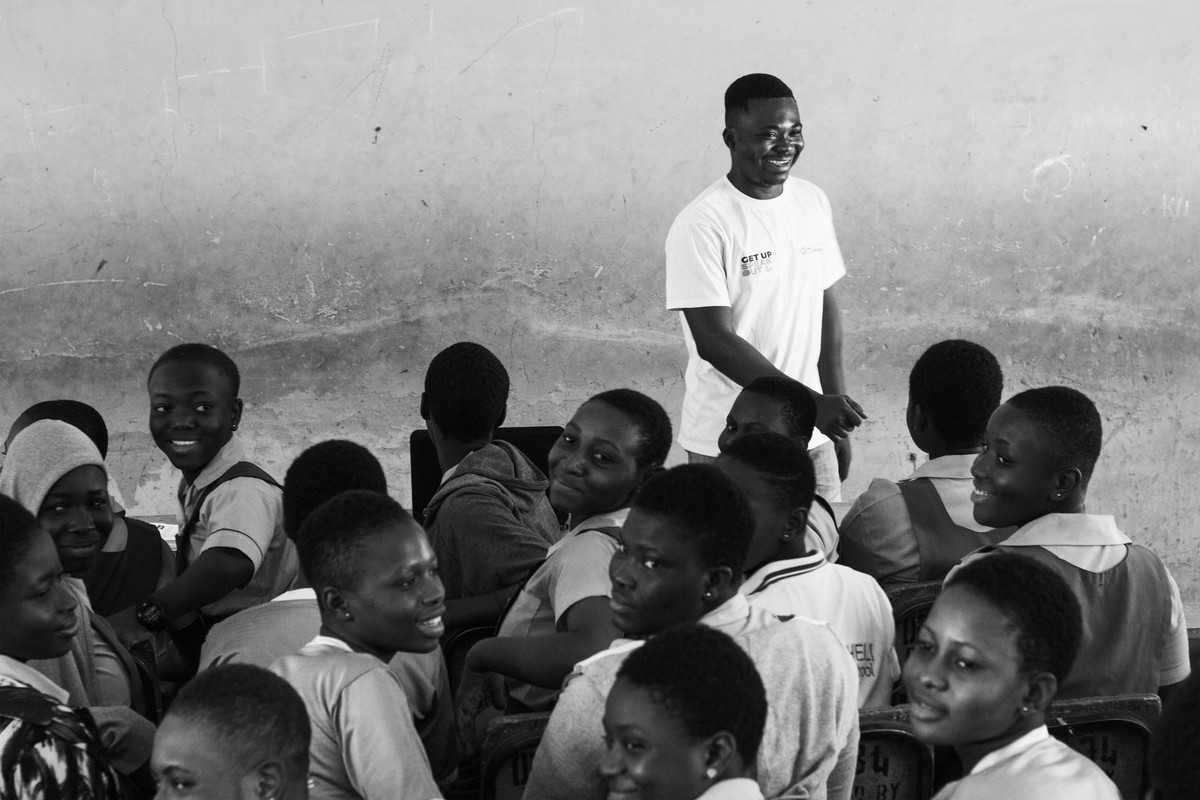
Engaging and empowering young women and adolescent girls to prevent the risks and mitigate the impact of HIV
Preventing HIV among adolescent girls and young women in sub Saharan Africa is critical if we are to end AIDS by 2030. We know that gender inequality increases HIV vulnerability of adolescent girls and young women and continues to be one of the least addressed bottlenecks fuelling the epidemic. A group of 179 young female champions from Malawi, Kenya and Uganda pioneered a gender equality approach to address the HIV burden in their countries. These girls used their agency, their skills to amplify their voices to address the heightened HIV vulnerability they and other girls like them face. They were part of a pilot project called ‘Empowerment + Engagement = Equality’ designed and implemented by UN Women and the International Planned Parenthood Federation (IPPF) to build a stronger agency and leadership of the young women and adolescent girls advocates, including those living with HIV, to engage in the national assessments initiated by the All In to End Adolescent AIDS platform. Through mentoring, capacity building, social media and peer support more than 1,000 advocates were mobilized and voiced their priorities at the local, national and global foras. The girls had safe spaces to come together, either through face to face meeting or WhatsApp groups to discuss not only about HIV but broader issues that affect gender inequality. They engaged with religious leaders, teachers and other community stakeholders to change harmful gender norms. ‘In the WhatsApp group we formed as Kenya advocates, we discuss issues affecting us like education, leadership, sexual and reproductive health and rights, HIV on a daily basis. We are drawn from different parts of the country, including Mombasa, Kisumu and Nairobi. I have never been to those places, but yet I feel so connected to them because of the friends. I have made and the similarity in the issues we talk about. In the WhatsApp group, we solve problems together, counsel each other, and motivate each other. But what has been amazing is the fact I have met fellow young ladies from two other African countries: Malawi and Uganda on WhatsApp! While WhatsApp gives us a good platform to come together as a core group of advocates our work goes beyond social media. We reach out to girls in and out of schools, talk to community leaders, teachers and parents about issues that affects HIV risks like child marriage, lack of girls education, sexual violence, HIV-related stigma. Through this advocacy work, I have discovered things about myself that I never knew I was capable of. I am now clearer about who I am and what I want for my life. I see that I am more confident in the way I speak and how I engage with people. I was previously a shy person who was fearful of talking to many people, but today, I am a confident young woman who is able to speak in public. Some of the most fulfilling work I have done as part of this project is support other girls like me to feel empowered and be in control of their lives. I share my personal experience and encourage girls living with HIV to believe that they too can walk with their heads held high and a smile on their face just like me ‘. Divina Kemunto,Kisii County, Kenya The young advocates mobilized over 1,000 girls and young women across the three countries, who reached out and made a real difference in the lives of thousands of other girls, including those living with HIV, by engaging with them, sharing information about HIV and the risk factors, mentoring and counselling them. They engaged with parents, teachers, community leaders, religious leaders, government stakeholders to amplify the risk factors that increase the girls’ vulnerability to HIV and advocate to address these at community and national level. For example, in Malawi the young advocates participated in a discussion with the first lady of Malawi, Her Excellency Dr. Gertrude Mutharik to share their concerns on HIV related stigma especially in school and health care settings for adolescents and young people, bottlenecks of girls continuing education, sexual and gender abased violence and child marriage. She committed to champion the causes of these young advocates, especially on addressing issues of gender based violence. These opportunities to engage at the high level panels increase the visibility of the HIV risks for young women and adolescent girls and the importance of tackling them if we are to end AIDS by 2030. The advocates continued to take their causes to global platforms. At the International AIDS conference in Durban, South Africa, the advocates highlighted the importance of recognising and addressing the critical linkages between gender-based violence and HIV. An empowered girl will reduce HIV risks because she will say no to early marriage; she can complete her education and have better economic prospects, she can negotiate for safe sex and prevent early pregnancies, she will know what to do if faced with sexual violence. An enabling environment, with no discriminatory laws and policies; and health systems and workers that respect young women and their access to services and rights to sexual and reproductive health; and communities that lift girls up and support their educational opportunities combined with empowered girls will contribute to ending AIDS. And when empowered girls have the skills to meaningfully engage with decision makers, policy makers and community stakeholders in an enabling environment, they will be powerful negotiators. Thus ensuring they are not left out when resources are allocated and strategies are developed to change the future of adolescent girls and young women… thereby paving the road to HIV prevention!

Resilience and survival in the camps of Nyala
Read more
Our staff never turn anyone away
At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am. From 8am we will be receiving a variety of clients for different services - whether post-abortion care, whether antenatal care - we have to give them all the services. We may end up to 10pm, because we'll never chase our clients, we'll never close the place when we have a client inside. People come when they have no hope. You receive them, and you give them hope by treating them properly and giving them quality services. The client gets better and will never forget you. And follow them up on the phone. "How are you doing?" It's good for us to know that they're doing well. Others even tell us 'The way you handle us, we love it so much'."; Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

Overview: A one-stop shop providing vital healthcare
Uganda has one of the highest fertility rates in the world, and as a result, it also has one of the most youthful populations - more than half of Ugandans are under the age of 15. Over 78% of the population is below the age of 30. The population is growing at a rate of more than 3% per year. Figures show that women – on average - give birth to two more children than they want. More than half of pregnancies in Uganda are unintended, and nearly a third of these end in abortion according to figures from the Guttmacher Institute. It also says that in Uganda approximately one in every 19 women has an abortion per year and with abortion being highly restricted most of these are unsafe. This rate is far higher than the average for East Africa and reflects the high level of unmet need for contraception in the country. Approximately, 755,000 unintended pregnancies occur annually out of which 297,000 result in unsafe abortions. Unintended pregnancy is common in Uganda, leading to high levels of unplanned births, unsafe abortions, and maternal injury and death. Women in the eastern and north regions had the highest proportions of unplanned births (50–54%) the high levels of unintended pregnancy and unplanned births in Uganda can be attributed primarily to nonuse of contraceptives by women who do not want a child soon. More than 80% of the population lives in rural areas. Millions of people still do not have access to a health clinic, and family planning, especially long term and permanent methods, is not available to the vast majority who live in rural and hard-to-reach areas. IPPF’s Member Association, Reproductive Health Uganda (RHU), is working hard on the ground to tackle these issues. It takes the approach that it offers people as many services as possible at its clinics so you can get your health needs met in the same place. This means you might go to a clinic for an HIV test but leave having being offered a range of contraception plus other tests for other sexually transmitted diseases or cancer. RHU has a network of clinics across the country and takes its services out to remote and rural areas through its mobile clinics. No one is left out by RHU. Whether people are poor or vulnerable or hard to reach, RHU makes sure they have access to all of the services they need. We visited one of RHU’s health facilities in northern Uganda to get a better idea of how our work makes a real difference to people and their lives. We wanted to hear stories about what difference getting contraception, counselling and testing meant in reality. For many people it is life-changing. Thousands of people go in and out of Gulu Clinic every year and thousands more get services through Gulu’s mobile clinics. Last year alone Gulu Clinic had 229,812 family planning clients and provided 769,707 sexual health services, 390,488 of those were to young people. It offers a ‘one-stop-shop’ approach which makes it easier for clients to get a range of integrated services. They can go to a clinic for a check-up but end up getting contraception, counselling and a whole range of other tests and treatments. These include family planning, infertility management, cervical cancer screening, cryotherapy, youth friendly services, sexually transmitted infections and general sexual and reproductive health (SRH). Denis Bongonyinge, who has worked at Gulu Clinic for four years, said: “For us our goal is to ensure that this place is just a one stop centre. When a client comes in, he goes out when he has got a very big package of services within the clinic. Even if we go out, we give very many services. Denis said he had come across a range of issues among the clients. Issues like high rates of teenage pregnancies, sexually transmitted infections and gender based violence which could all be dealt with at the centre. He added that he believed Gulu had managed to offer such a range of services because of its willingness to work with other partners interested in scaling up uptake of family planning and generally sexual and reproductive health services. Gulu Clinic is also inclusive to a wide range of people across the community and this includes sex workers and disabled people. Vicky Acora is deaf and has had problems getting services at other hospitals. But, she says about RHU: “They are really most welcoming and they try to communicate even in the little sign language they know. They are really very warm” She says she has since been advising other deaf persons to seek services at Reproductive Health Uganda because of the quick services. “I encourage other people to come here because it is fairer. I encourage other disabled people who use wheelchairs not only the deaf to come and access services here because it is really accessible for those who have a disability.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

A sex worker's story
"I’m 25-years-old and a mother of two children. I lost my parents during the war, so I grew up alone. I ended up dropping out of school and I went for sex working. I am selling myself in order for me to sustain a living. "My second born is 10 months old and my first born is 7 years. He’s at home with me because I have no money to pay for his school fees. "I heard about Reproductive Health Uganda a few years ago but I couldn’t access it until they did their outreaches where I was staying. I stay far from town. "I came purposely here to RHU for Hepatitis B testing and also counselling because I have so many personal problems. I’m also on family planning and about to start using an IUD, I want to get that from here now also. "I like coming here, I’m satisfied with all the services because it's free of charge, they’re so caring, the way that they handle people. They handled us in a good way, they know how to talk to us. I’m so happy about the way I was welcomed here. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
Pagination
- Previous page
- Page 10
- Next page






